For anyone, choosing the right method of birth control presents a challenge. This challenge becomes even greater for female endurance athletes, as different methods have different pros and cons related to health and athletic performance. I’ve spent the last couple of months learning about the pros and cons of various contraceptive methods as I’ve debated whether to switch up my routine, and this post summarizes what I’ve learned about contraception and its effects on athletic performance. I should caveat this post with the disclaimers that (1) I’m not a doctor, (2) I have received no formal medical training (although this post has been checked and edited by multiple nearly-doctors and female badasses in my corner—you know who you are and thank you!), and (3) contraception choices are very individual-specific and have no “right” answers. You should absolutely do your own research and make an informed decision about what is best for you!
Combined oral contraceptive pills (OCPs): OCPs deliver estrogen and progesterone systemically (i.e., throughout the body). A big pro is that it is easy to stop taking them for any reason without going through a medical procedure (such as IUD removal). However, some important cons for female athletes are that OCPs have been linked to worse athletic performance outcomes, including decreased VO2 max, higher oxidative stress, and/or decreased ability to adapt to intense training. This is largely because estrogen changes the body’s ability to hit intensities and recover from stress. Since OCPs pump a large amount of estrogen and progesterone through the body throughout the month (approximately 6-8 times the amount we produce naturally), women are effectively in a continuous high-hormone state and miss out on the natural fluctuations in hormones that generally allow them to hit higher intensities in the first half of their cycle (the follicular or low-hormone phase). When female athletes use OCPs, experts estimate that around 11% of their performance potential is left on the table.
Moreover, an important misconception about OCPs is that they give you a natural period. There is a “withdrawal bleed” associated with the fourth week of the cycle (a placebo pill), but this bleed is not a normal period and does not indicate that a woman is cycling naturally on her own. This is why using OCPs for female athletes experiencing hypothalamic amenorrhea (stopped periods) is generally a bad idea (unless it is being used to treat other underlying health conditions such as endometriosis, PCOS, chronic pelvic pain, menstrual migraines, premenstrual dysphoric disorder, ovarian cysts, acne, or hyperandrogenism), because it masks the underlying problem of energy deficiency and may not fix the associated declines in bone density and other negative health outcomes.
Note: Other options that include systemic hormones are the patch, the DePo-Provera injection, and the implant. There is less research on how these methods impact female athletes and endurance training given their often less-desired side effect profile, but there is reason to believe that they have similar systemic effects on performance.
Hormonal IUDs (in a class known as long acting reversible contraceptives (LARCs); brands include Mirena, Kyleena, Liletta, Skyla, etc.): Hormonal IUDs (intrauterine devices) are small, T-shaped devices that are inserted vaginally and placed directly inside the uterus by a medical provider. Hormonal IUDs release small amounts of the hormone progestin (levonorgestrel) into your body, which prevents pregnancy by stopping sperm from reaching and fertilizing eggs via changes to cervical fluid that inhibit sperm transport and changes to the endometrium that inhibit implantation, among other mechanisms. Pros are that they are highly effective, can be used for 5-7 years, and do not release estrogen into the body, so they are not associated with the same negative effects on athletic performance as combined OCPs. By contrast, research suggests that they mimic a natural cycle and might even be beneficial at reducing PMS-related performance declines in the late luteal phase. Fertility also usually resumes immediately after IUD removal, while it can take longer to resume when coming off of combined OCPs and other systemic methods.
However, important cons for female endurance athletes who are training at a high level and/or are worried about potential energy deficiency are that they can lead to stopped periods, which eliminates a key indicator that an athlete is handling fueling, training, and stress appropriately. (Note: This can also be a pro for those who are not worried about energy deficiency and prefer the logistical benefits of not dealing with a period.) The differences between hormonal IUD brands are the size (for example, Mirena and Liletta are slightly larger than Kyleena and Sykla) and the amount of hormones that are released into the body. For the Mirena, for example, which has 52 mg of levonorgestrel, about 20% of women will stop getting their period after a year, and for the Kyleena, which has 19.5 mg of levonorgestrel, about 12% will stop their period. There is currently no way to predict how a woman’s cycle will react to a hormonal IUD, but it’s important to keep in mind that IUDs can be removed. It also takes people a few months to adjust to the influx of hormones that come from the IUD, so cycles can be irregular and many people experience spotting as they adjust. People usually have their new normal cycle by 3-6 months.
Finally, IUD insertion can also be painful. That said, there are a variety of things you can do to mitigate this, including asking for lidocaine-prilocaine cream, taking misoprostol prior to insertion (though the data are mixed on whether this helps), using ibuprofen for cramping, and scheduling your training around the insertion procedure to give your body a chance to rest and do its thing. Many women agree that a small amount of discomfort is worth it for the peace of mind that they will not get pregnant.
Progestin-only mini pill: For women who do not want the systemic effects of estrogen and progesterone but also do not want an IUD, there are progestin-only oral contraceptives. These pills are thought to have similar non-effects on athletic performance as an IUD and are easier to stop taking for any reason, although they are not localized.
Copper IUDs (also a LARC; most common brand is Paragard): The copper IUD (Paragard) is a hormone-free IUD that works by creating a toxic environment in the uterus for sperm. It is one of the only hormone-free birth control options for women (other than medical sterilization and FAM) and is highly effective. It can also be inserted as an emergency contraceptive method, and is effective for up to 10 years. A big pro is that you will still get a period while using a copper IUD (allowing you to use your period as a guide for health and performance), but a con is that periods can generally be heavier or more painful for several months after insertion. Like with hormonal IUDs, the insertion procedure can also be painful, and the copper IUDs are the largest in terms of size (although they are still objectively small and do not interfere with athletic performance or sex).
Fertility awareness method (e.g., Natural Cycles): Some people prefer to avoid hormones and devices altogether and will use the “fertility awareness method” to track their cycles and prevent pregnancy. By tracking indicators like basal body temperature, cervical fluid consistency, and cervical shape, you can identify with some certainty what phase of the menstrual cycle you are in and avoid unprotected sex during your fertility window, which can be about 7-10 days for most people. Apps like the Natural Cycles app have made tracking easier, and many women enjoy learning more about their own physiology throughout the process. However, this method does take a lot of effort and tracking behaviors, and it rules out unprotected sex for several days in a given month, which many people dislike.
My experience
My main considerations related to choosing a birth control option were the following: (1) I probably want to get pregnant eventually, but not anytime soon, and I want to have high confidence that I won’t get pregnant now; (2) I do not want birth control to negatively impact my athletic performance; and (3) I like to use a natural menstrual cycle as a regular indicator that my body is handling stressors, training load (energy output), and fueling (energy input) appropriately. As someone who experienced RED-S (relative energy deficiency in sport) in college (you can read more about that here), point #3 was particularly important to me.
For all of these reasons, not being on birth control and tracking my cycle naturally was the right choice for me for a while—that is, until I confronted the reality that condoms aren’t perfect and had to take plan B (an emergency contraceptive). While that was ultimately the right decision, it was an objectively bad experience for me for multiple reasons (happy to elaborate for anyone in a similar position who is curious), and I was confident that I didn’t want to have to take plan B again unless absolutely necessary. So that meant that I needed to find a new birth control solution that would give me greater certainty that I could avoid an unwanted pregnancy.
I was fairly certain that all methods that featured systemic (non-localized) doses of estrogen and progesterone (including OCPs, patches, injections, implants, etc.) were off the table for me because of their potentially negative consequences on athletic performance. That left me with hormonal IUDs, a copper IUD, or the fertility awareness method. FAM seemed like a lot of work to do correctly, and I was worried that I would not feel as confident about the effectiveness of the method as I would with an IUD.
The copper IUD was attractive to me because it contains no hormones, but I was concerned about the performance effects (and logistical nuisance) of potentially heavier, longer, and more painful periods—especially when I’m well on my way into a big IRONMAN build. I actually sent Colleen Quigley—an Olympic steeplechaser-turned-triathlete and social media influencer who has been amazingly vocal about her copper IUD experience—an Instagram DM asking for her thoughts, and she reiterated that she loves the copper IUD now but would recommend getting it placed during an off season rather than during peak training, which wouldn’t have been an option for me until the fall.
For the hormonal IUDs, my main hesitation was the idea that I could end up not getting my period, which would make it harder to have an objective indicator of overall health and balanced energy input and output. Ultimately, I decided to go with the Kyleena, one of the two lower-dose hormonal option (my OB-GYN told me that the Skyla, which is technically the smallest and lowest hormone dose, is being phased out of use because it’s not very different from the Kyleena and only lasts for three years before it has to be removed or exchanged). I then learned more about ways to keep tabs on your cycle even without having your period as an indicator, including:
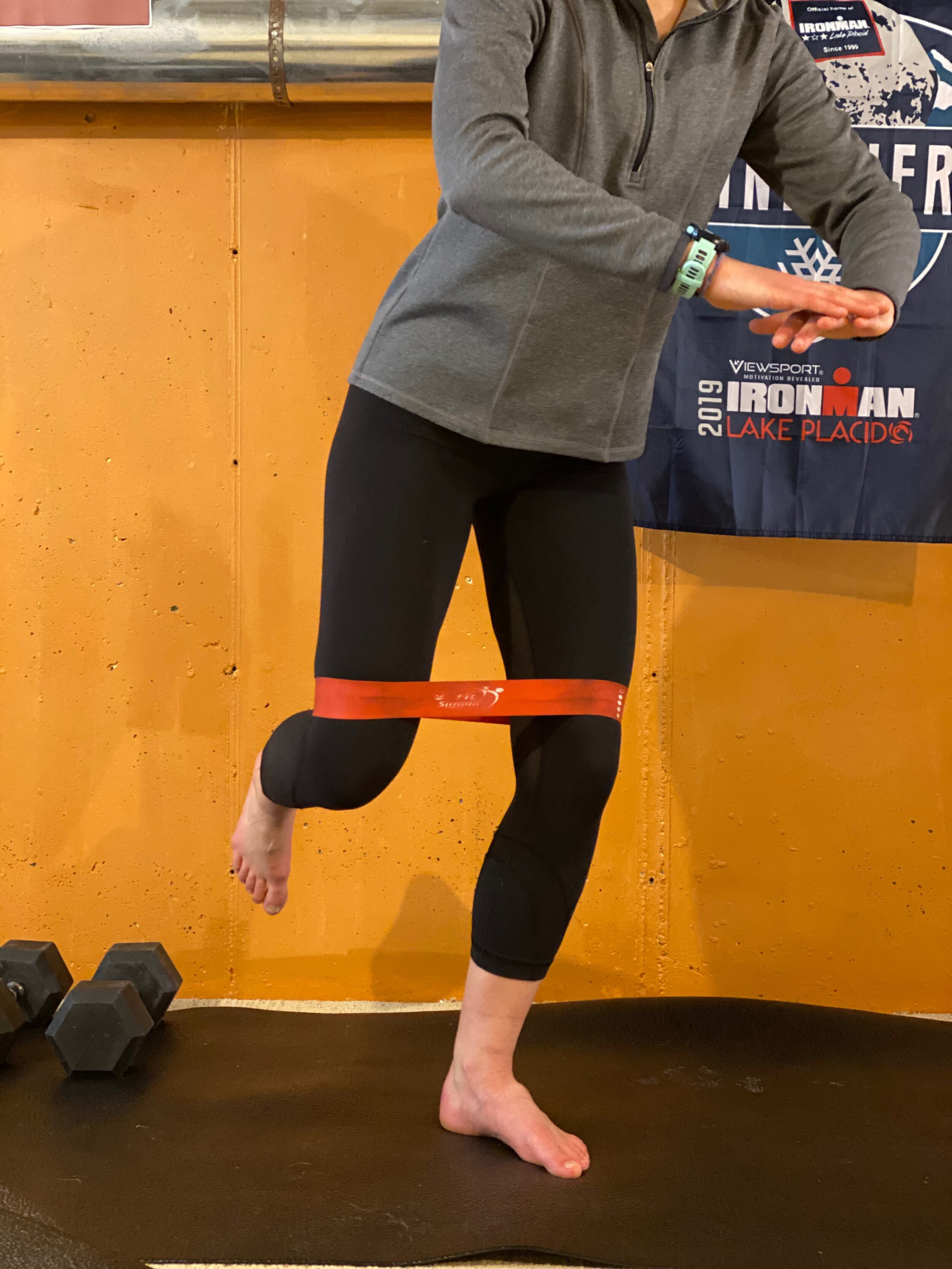
Keeping track of other menstrual cycle-related symptoms, including patterns in resting heart rate or heart rate variability, breast tenderness, feeling more bloated (a result of fluid retention), mood swings, sex drive, cervical fluid, etc.
Keeping track of symptoms related to energy balance, including weight loss, mood swings (especially anxiety/depression), persistent illness, injuries, sleep quality, performance declines, always feeling cold, etc.
Optionally, getting bloodwork done to measure estrogen, progesterone, and testosterone to let you know whether you are in the follicular or mid-follicular phase.
The insertion procedure itself was not fun at all, which is another important potential con for people considering getting an IUD. I had heard that the Kyleena insertion might be the least painful (compared to the Mirena or the Paragard) because it is the smallest in size, but holy hell it was an experience. I took misoprostol the night before the procedure, which is theoretically supposed to make insertion less painful by dilating the cervix. I also took ibuprofen about 30 minutes before the procedure and throughout the day afterwards, and I had planned a very easy training day. Even so, my OB-GYN had to do the insertion twice because according to her I have “the strongest pelvic floor she has ever seen” (humble brag, I know) and it hurt a lot both during and afterwards. But I woke up the next day feeling a lot better and have only experienced mild cramping and other PMS-like symptoms in the days following, and have mostly resumed normal training.
I’ll have to do a follow-up post in a few months to definitively weigh in on how the IUD did or did not affect my experience as a female athlete, but for now, I stand by the decision that I made. I know that my odds of getting pregnant are extremely unlikely, I am confident that the IUD is unlikely to negatively impact my performance, and I have a plan for how to stay on top of health indicators even if I end up in the minority of people with an IUD that do not get a period. I also feel empowered for making an informed decision. Special thanks to the many amazing friends, doctors, and other important women in my corner who shared their experience, expertise, and insight to help me figure this out—girl power!
Some resources if you want to learn more about contraceptive methods and pros/cons:
The Effects of Contraception on Female Athletes’ Performance
The Fifth Vital Sign: Master Your Cycles & Optimize Your Fertility
A few favorite social media follows on topics related to contraception/ the menstrual cycle and female athletes: